News
Trump’s “One Big Beautiful Bill” (OBBB), passed on July 4, 2025, initially promised significant changes to Health Savings Accounts (HSAs). However, the final version of the legislation contained modest updates to HSA policy. Current HSA holders get to keep what they have, but significant reforms such as extending eligibility to those on Medicare or relaxing contribution restrictions, were abandoned in negotiations. Instead, the bill primarily focuses on restructuring Medicaid and welfare programs, implementing work mandates, and providing tax credits tied to families and newborn savings accounts.
Health Saving Accounts were thought to have a larger presence in the bill that would have placed HSAs as a centerpiece of healthcare funding and provided areas for growth by softening regulations of who can contribute, such as those on Medicare Part A. Without eligibility expansion, HSAs remain mostly unchanged, and tax-advantaged growth remains limited to current users.
Here’s a breakdown of what changes OBBB brings to HSA plans:
- If you are enrolled in a Bronze or Catastrophic ACA plan, you are now eligible to contribute to HSAs starting January 1, 2026.
- HSA funds can be used for Direct Primary Care (DPC) arrangements. DPCs typically follow the model of a monthly fee, which covers office visits prior to meeting the HDHP deductible. With OBBB, these monthly fees now fall under qualified HSA expenses if they do not exceed $150/month for an individual or $300/month for families.
- First-dollar coverage for telehealth services no longer disqualifies HSA status, which allows plans to provide low or no-cost telehealth services before satisfying your deductible if you are enrolled in a qualified HDHP without using your HSA contributions.
HSAs remain a useful tool for eligible taxpayers and serve as a tax-savings vehicle.
Triple Tax Advantage
- Pre-tax Contributions – Money goes in tax-free, reducing your taxable income
- Tax-free Growth – Funds grow tax-deferred through interest and/or investments (no capital gains)
- Tax-Free Withdrawals – As long as funds are used for qualified medical expenses, withdrawals are tax-free
Saving for the Future
- You can invest your HSA balance (once you hit a threshold set by your carrier, allowing it to grow like a retirement account)
- Can be used in retirement tax-free for medical expenses, or after age 65, for any reason (income taxes apply only if not used for qualifying healthcare expenses)
HSA funds roll over year-to-year, and don’t have a use-it-or-lose-it rule like Flexible Spending Accounts (FSAs). Additionally, you can use your HSA funds for a wide range of expenses, including copays, prescriptions, dental and vision care, mental health services, and certain over-the-counter items (such as pain relievers, allergy medications, and first-aid supplies). Lastly, you OWN your HSA – it stays with you if you change jobs or retire. You control how and when it is used, allowing you to learn how they work and ensure you make the most out of the account.
While the “One Big Beautiful Bill” fell short of delivering the HSA expansion many had hoped for, it did make some notable improvements. It’s clear that Health Savings Accounts remain one of the most innovative tools for managing healthcare costs, both now and in the future. In today’s uncertain and costly healthcare environment, understanding and maximizing your HSA is essential. For those enrolled in an HSA, remember, it isn’t just a spending account — it’s a strategy.
Posted by CalCPA Health | July 2025
July is UV Safety Awareness Month, and it’s the perfect time to remind ourselves how important it is to protect our skin from the sun’s harmful ultraviolet (UV) rays.
Individuals with fair skin can sunburn in as little as 10-15 minutes of midday sun exposure when UV rays are the highest. UV rays are typically high between 10 a.m. and 4 p.m. and the highest around 11 a.m. to 1 p.m. Don’t let a cloudy day fool you because UV rays can be just as intense as on a sunny day.
What Are UV Rays?
Ultraviolet radiation from the sun comes in three forms:
- UVA rays penetrate deep into the skin and are responsible for premature aging, such as wrinkles and age spots, and can contribute to skin cancer.
- UVB rays are more intense and damage the outer layers of the skin, causing sunburns, and they play a key role in the development of most skin cancers.
- UVC rays are the most dangerous, but they are absorbed by the Earth’s atmosphere and don’t typically pose a threat during everyday sun exposure.
Types of Skin Cancer
Skin cancer is the most common cancer in the U.S., but it’s also one of the most preventable. Here are the three main types:
- Basal Cell Carcinoma (BCC): The most common and least aggressive type, accounting for approximately 80 percent of all cases*. It often appears as a flesh-colored bump or pink patch of skin and may bleed or form a scab. BCC grows slowly and rarely spreads, but it can cause local tissue damage if untreated.
- Squamous Cell Carcinoma (SCC): Accounts for approximately 20 percent of all skin cancer cases* and tends to occur on areas of the body most exposed to the sun, such as the face, neck, and hands. SCC shows up as a scaly red patch, a wart-like growth, or a sore that won’t heal. It can grow deeper and, in some cases, spread to other parts of the body.
- Melanoma: The most serious form of skin cancer, which accounts for about four percent of skin cancer cases*. Melanoma can develop from an existing mole or appear as a new dark spot. Early detection is critical since melanoma can spread quickly and be life-threatening if not caught early.
How to Protect Yourself
- Wear sunscreen every day with broad-spectrum (UVA/UVB) protection, SPF 30 or higher.
- Cover up with clothing, hats, and sunglasses that block UV rays.
- Seek shade between 10 a.m. and 4 p.m., when the sun’s rays are strongest.
- Avoid tanning beds, which emit concentrated UVA and UVB radiation.
Check Your Skin
Examine your skin regularly for changes in moles, new growths, or sores that don’t heal. When in doubt, get it checked out. Annual skin exams with a dermatologist are a smart step in preventing skin issues, and early detection is key. Protecting your skin today is an investment in your health tomorrow. Enjoy the sunshine safely.
* https://skinandcancerinstitute.com/july-is-uv-safety-month/
What is the name of your health plan? Who’s your insurance carrier? If you had to look it up right now to check, you’re not alone; many people are not sure. If you don’t know the basics, you won’t be able to take full advantage of your benefits.
Health insurance is a tool—but only if you know how to use it. You don’t want to be like so many people out there who experience a health emergency and must deal with the stress of not understanding their health care coverage in a time of trauma.
Knowing your health plan matters
Surprise Bills
- You may get a procedure for which you need pre-authorization, and did not know until you received an unexpected bill. This happens more often than you can imagine.
- If you don’t know whether your provider is in-network or out-of-network, or how your plan covers care, you are more likely to pay out-of-pocket for services that should have been covered.
Miss Out on Preventive Services
- Many plans offer 100% coverage for preventive services (such as mammograms, colonoscopies, and annual physicals), virtual visits, and wellness programs. But you can’t use benefits you don’t know you have.
You Can’t Advocate for Yourself Without the Basics
- Here are just a few of the ways understanding your plan helps you:
- Ask the right questions and go through the proper channels for care; reach out for help by calling your insurance provider
- Spot billing errors
- Take advantage of telehealth, HSA options, or mental health coverage (to name a few)
What You Need to Know – Today
At the very least, every health insurance subscriber should know:
- Your carrier (the company providing your insurance, such as Anthem, Delta Dental, and VSP)
- Your plan type (Health Maintenance Organization – HMO, Preferred Provider Organization – PPO, Exclusive Provider Organization – EPO, or Health Savings Account – HSA)
- Whether your plan is individual, employer-sponsored, or part of an association
How to Find These Items Quickly
- Check your insurance ID card – it typically lists the plan name and carrier
- Log in to your carrier’s member portal (the website usually is on the ID card) – this is where you will find your plan documents, benefits, and provider network information
- Download your carrier’s app and create an account so that you have access to your ID card at all times, as well as to your health and benefit information and plan summary (Summary of Benefits and Coverage – SBC)
- Ask your HR or firm administrator if you’re part of an employer or association plan
Then, take a few minutes to review your SBC, as it outlines the services that are covered, excluded, and the pre-authorization requirements. It also helps you understand what your plan will cover and what you may need to pay out-of-pocket for. Knowing the basics gives you power as a healthcare consumer and enables you to become your own best advocate.
Please don’t wait for an emergency to try and understand your health plan; familiarizing yourself with it now is a smart way to save time, avoid stress, and ensure you get the most from your benefits.
*********
Created by CalCPA in 1959 as The Group Insurance Trust of the California Society of CPAs, CalCPA Health has remained steadfast in its mission to provide quality “boutique style” health care solutions—from medical, dental and vision to life and long-term disability—with unparalleled convenience and stability. It helps ensure that members can navigate the challenges of health care with confidence and peace of mind. CalCPA Health offers exclusive health and benefit plans to members, and there is a high level of trust knowing that these plans are operated by individuals who understand the unique needs of the profession – CalCPA members.
The IRS recently released the contribution limits for Health Savings Accounts (HSAs) for 2026. In the upcoming year, we will see an HSA contribution limit increase to $4,400 for individuals and an increase to $8,750 for a family. The IRS implemented inflation-adjusted parameters for health savings accounts in Revenue Procedure 2025-19.
For 2026, individuals with self-only coverage can contribute up to $4,400 to their HSAs, up from $4,300 in 2025. Family plans can contribute up to $8,750, up from $8,550 in 2025. The IRS also noted that the 2026 catch-up contribution for those aged 55 and older will remain $1,000 for 2026, unchanged from 2025.
According to Fidelity Investments’ 2024 Retiree Health Care Cost Estimate, a single 65-year-old retiring can expect to spend an average of $165,000, or $330,000 per couple, in health care and medical expenses throughout retirement. These figures are up nearly 5% over 2023 and more than doubled from the first estimate in 2002. Understanding how to save and invest with an HSA plan is key to helping you plan for future expected and unexpected medical expenses.
If you are in an HSA and have questions about how to get the most out of the plan, CalCPA Health can help answer your questions. CalCPA Health is at the forefront of HSA adoption, offering the most HSA plan options in California. CalCPA members have a strong understanding of the tax benefits HSAs provide. Education is key, and CalCPA Health is here to help whether or not you are in one of our plans. We are a resource for you, so please feel free to ask questions by emailing info@calcpahealth.com.
 The eMagazine dedicated to improving members’ well-being
The eMagazine dedicated to improving members’ well-being
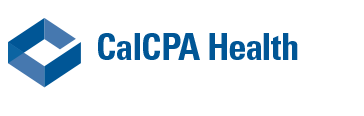
- Heart Boosters
- Helping Your Child Use Medication
- Home Medical Test Pros and Cons
- ASK THE DIETITIAN: Freezing Food
- Recipe – One-Pot Chicken Stew
In each issue you will find information and inspiration to help you with your health and wellness goals.
 The eMagazine dedicated to improving members’ well-being
The eMagazine dedicated to improving members’ well-being
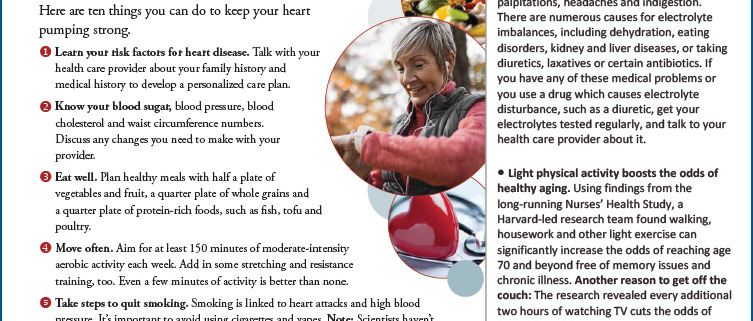
- Health Fads You Don’t Need
- The Toll of Financial Stress
- Sleep and Mood
- The Science of Satiety
- Prebiotic Soft Drinks
- Recipe – Sheet Pan Honey-Mustard Chicken
- What is norovirus?
In each issue you will find information and inspiration to help you with your health and wellness goals.
 The eMagazine dedicated to improving members’ well-being
The eMagazine dedicated to improving members’ well-being
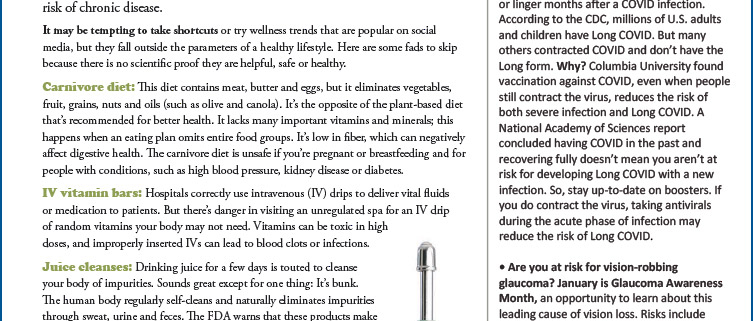
- Reverse Type 2 Diabetes?
- Video game addiction?
- Your Personal Exercise Plan
- Jazz Up Your Breakfast
- Ultra-Processed Foods and Long-Term Health
In each issue you will find information and inspiration to help you with your health and wellness goals.
 The eMagazine dedicated to improving members’ well-being
The eMagazine dedicated to improving members’ well-being
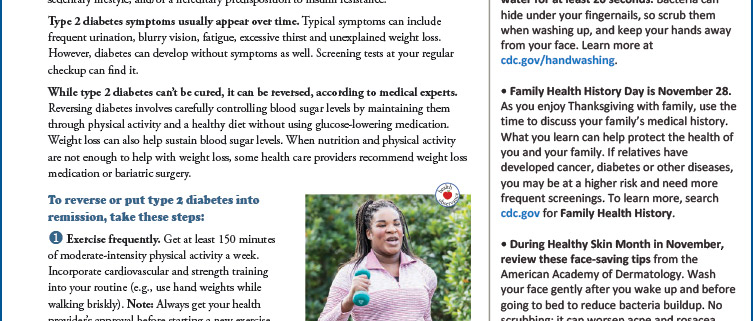
- When to Get a Second Opinion
- Protect Your Teeth
- Exercise Guidelines
- What is a diagnostic mammogram?
- Plant-Based Proteins
In each issue you will find information and inspiration to help you with your health and wellness goals.
 The eMagazine dedicated to improving members’ well-being
The eMagazine dedicated to improving members’ well-being
- Lower Your Risk: Metabolic Syndrome
- Study: Long COVID
- Time-Restricted Eating: Heart Disease Risk
- Ancient Grains, Modern Nutrition
- Does Caffeine Cause Stress?
In each issue you will find information and inspiration to help you with your health and wellness goals.
In this podcast, we learn what inner peace is and how it is different for each of us. We all have different journeys in life, and inner peace means we accept our flaws – our strengths – and accept who we are as a unique individual. Self-awareness and managing our thoughts and emotions – to help us achieve a balanced state of mind. Taking the time to understand our feelings, to let go of anger and guilt, and acknowledging that life is full of uncertainty helps us to move forward and not get hung up on negative thought patterns. Staying away from negative self-talk, being kind to others, being kind to yourself, and making sure that you take time for yourself each day to focus on relaxation, meditation, or a walk outside all help contribute to your overall well-being.
This podcast is for informational purposes only and should not be considered legal health or medical advice. CalCPA Health is not affiliated with Balancing Life Issues. The podcasts are provided by Balancing Life Issues to provide possible resources and helpful information.